![]() +65 6239 5231 (Parkway East Branch)
+65 6239 5231 (Parkway East Branch)
![]() +65 9722 6526 (For Eye Appointment)
+65 9722 6526 (For Eye Appointment)![]() +65 8508 9033 (For ENT Appointment)
+65 8508 9033 (For ENT Appointment)
![]() eyeinfo@ceec.com.sg
eyeinfo@ceec.com.sg![]() entinfo@ceec.com.sg
entinfo@ceec.com.sg
![]() +65 6339 8938
+65 6339 8938
- Myopia, hyperopia, astigmatism
- Myopia control eye drops
- Lazy eye (“amblyopia”)
- Paediatric vision screening
- Clues that your child can't see well
- Frequent blinking and tearing
- Tear duct obstruction
- Squint (eye misalignment)
- Droopy eyelids
- Colour blindness
- Spectacle fitting
- Eye infections or allergy
- Paediatric cataract & cataract surgery
- Pediatric glaucoma
- Retinopathy of prematurity
ENQUIRY FORM
Retinopathy Of Prematurity
What is retinopathy of prematurity?
Retinopathy of prematurity (ROP) is a potentially blinding eye disorder that can affect premature infants weighing 1500 grams or less, who are born before 32 weeks of gestation. (A full-term pregnancy has a gestation of 38–42 weeks). The smaller the baby is at birth, the more likely he/she will develop ROP. ROP affects the growing blood vessels in the light-sensitive layer at the back of the eye (retina).
Why does ROP develop?
In a full term infant, the growth of normal blood vessels in the retina is almost complete at birth.
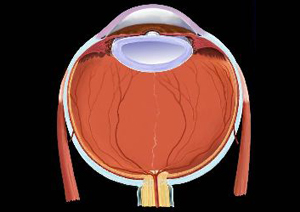
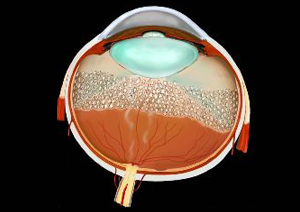
Full term eye with fully developed retina
In premature infants, as the baby is not in the natural environment of the mother’s womb, retinal blood vessels swell and may grow abnormally or excessively. When the condition is advanced, these abnormal retinal vessels extend into the jelly-like substance (vitreous) that fills the centre of the eye. Bleeding from these vessels may scar the retina and cause retinal detachment, which is a serious blinding condition if not treated promptly.
Do all premature infants develop ROP?
Today, with advances in neonatal care, smaller and more premature infants are being saved. Therefore, more babies are being screened for ROP. However, not all infants born premature develop ROP. The group at risk of developing ROP are those who weigh 1500 grams or less at birth, or are born before 32 weeks of gestation. The more premature, sick and low birth weight the infants, the higher the risk of developing ROP.
How does the doctor screen the infant’s eyes for ROP?
Premature infants who fall into the criteria for screening, are usually examined approximately 4-6 weeks after birth. Eye drops are instilled to enlarge the pupils so that the paediatric ophthalmologist, using special equipment, can have a good view of the back of the eye i.e. the retina.
How does ROP progress?
ROP is classified by zones and severity. The lower the zone (i.e. zone I), the closer the abnormal vessels are to the centre of the retina, and therefore the higher the threat to vision. ROP severity is classified into 5 stages, with stage 1 being the mildest form and stage 5 being the most severe. At each stage, the presence of “plus” disease is also documented. Plus disease is a clinical picture of engorgement and tortuosity of the blood vessels of the retina, and generally indicates a rapidly progressive course and an urgent need for treatment.
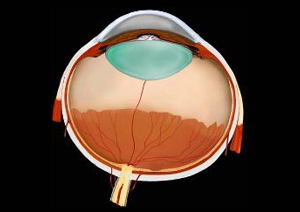
Stage 1 ROP
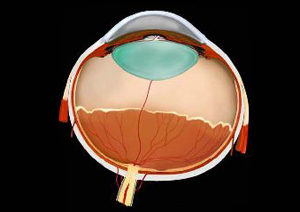
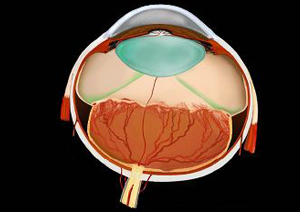
Stage 2 ROP
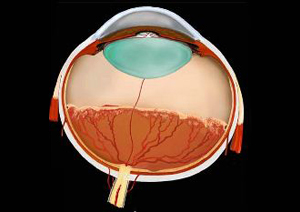
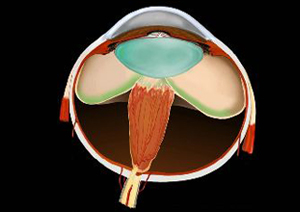
Stage 3 ROP
How is ROP treated?
The mild stages (i.e. Stage 1-2) do not require intervention except for close monitoring by the paediatric ophthalmologist. Stage 3 ROP in zone 1 or Stage 3 ROP with plus disease require treatment. Laser treatment, consisting of treating the abnormal peripheral retina with tiny laser burns, is the standard treatment for advanced ROP.
Post-laser treatment with disappearance of abnormal vessels
When retinal detachment occurs, the disease is classified as Stage 4-5 ROP. Advanced stage ROP is uncommon if screening and timely treatment are practised. Retinal detachment surgery is often required if a child presents with Stage 4-5 ROP.
Stage 4 ROP with partial retinal detachment
Stage 5 ROP with total retinal detachment
What happens if treatment does not work?
While ROP laser treatment decreases the chances of progression to the advanced stages, it does not always prevent vision loss. Unfortunately, a small percentage of premature and very sick infants, despite timely monitoring and intervention, continue progressing to blindness. It is therefore important not to default on follow up eye visits for ROP.
What are the long term problems for babies with ROP?
Ex premature babies are at higher risk of developing short-sightedness, astigmatism, squints and lazy eye. Ex premature children with ROP have a higher risk of getting the above mentioned problems than ex prems without ROP. Therefore, children with ROP need regular eye exams, even after the ROP has resolved.
![]() Mt Elizabeth Novena Specialist Centre
Mt Elizabeth Novena Specialist Centre
38 Irrawaddy Road, #10-21/39/40
Singapore 329563
WA: 8508 9033 | TEL: 6339 8938
EMAIL: info@ceec.com.sg
8:30am - 5pm (Mon- Fri)
8:30am - 12.30pm (Sat)
PH & Sunday: CLOSED
![]() Parkway East Hospital
Parkway East Hospital
321 Joo Chiat Road, #03-01
Singapore 427990
WA: 8504 6368 | TEL: 6239 5228
EMAIL: info@ceec.com.sg
8:30am - 5pm (Mon- Fri)
8:30am - 12pm (Sat)
PH & Sunday: CLOSED
![]() Mt Alvernia Medical Centre
Mt Alvernia Medical Centre
820 Thomson Road, #07-65
Singapore 574623
WA: 8508 9033 | TEL: 6258 8638
EMAIL: info@ceec.com.sg
8:30am - 5pm (Mon- Fri)
8:30am - 12pm (Sat)
PH & Sunday: CLOSED
- Myopia, hyperopia, astigmatism
- Myopia control eye drops
- Lazy eye (“amblyopia”)
- Paediatric vision screening
- Clues that your child can't see well
- Frequent blinking and tearing
- Tear duct obstruction
- Squint (eye misalignment)
- Droopy eyelids
- Colour blindness
- Spectacle fitting
- Eye infections or allergy
- Paediatric cataract & cataract surgery
- Pediatric glaucoma
- Retinopathy of prematurity

